
newborns 1
Michael Ferguson, MD, MTeach, demonstrating the augmented reality simulation of a newborn in distress. Photo: Black Fly Media
“If you don’t regularly employ these complex therapeutic methods, it’s going to be difficult to use the skills when the time comes,” says Mary Ottolini, MD, MPH, MEd, the George W. Hallett, MD, Chair of Pediatrics at the Barbara Bush Children’s Hospital at Maine Medical Center.
“Clinicians have great ideas but no clue about how to move them forward toward an actual product or service. The Innovation Center steered me in the right direction, helping me iterate on the idea, applying for grant funding, and answering questions like: How do I pitch this? What do I say?”
— Michael Ferguson, MD, MTeach, Pediatric Intensivist, The Barbara Bush Children’s Hospital at Maine Medical Center
Inspired by the work of Alexa Craig, MD, MSc, a researcher and neurologist with Maine Medical Partners, Mary and her colleague Michael Ferguson, MD, MTeach, decided they needed to do something to support rural healthcare workers and their newborn patients. Dr. Craig studies the detection of and treatment for neonatal encephalopathy in rural areas. She’s developing monitoring devices with smart technology to determine if newborns in distress need therapeutic hypothermia, or “brain cooling,” the only known treatment for the condition. When every second can mean the loss of brain tissue, providers need to act quickly and confidently.
In rural communities where cases of neonatal distress occur only once or twice a year, staff are not always comfortable using these lifesaving tools. Mary and Michael knew they wanted to tackle this problem head on.
“MaineHealth Innovation provided a safety net for our idea to get this training where it is needed most.”
— Mary Ottolini, MD, MPH, MEd, George W. Hallett, MD, Chair of Pediatrics, The Barbara Bush Children’s Hospital at Maine Medical Center
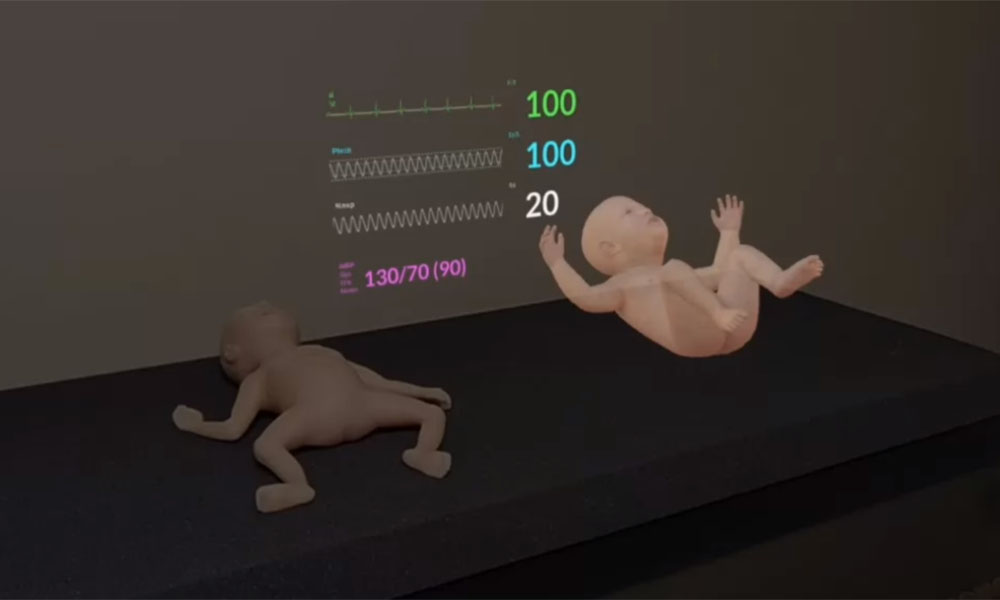
A physical neonatal simulation manikin (left) and the augmented reality overlay (right), as seen through Hololens goggles
The two set out to mobilize neonatal distress simulation training in rural Maine communities. Through a connection made by MaineHealth Innovation, they partnered with Case Western Reserve University (CWRU), leaders in augmented reality, to develop the specific software needed to simulate a real-time neonatal distress scenario. Shortly after, their “Augmented Technology for Medical Simulation” (ARTforMS) innovation was selected to receive $20,000 from the inaugural MaineHealth Innovation Ignite Fund.
The funds were used to purchase a suite of equipment to create what Michael refers to as “simulation in a suitcase.” ARTforMS uses the Microsoft Hololens mixed reality goggles, Empatica bio-sensing wrist watches and CWRU’s special augmented reality software to project the simulated scenario and allow the trainee and instructor to react to the same image, giving rural healthcare professionals the life-like training they need to recognize and react to these infrequent, but life-threatening, instances of infant distress.
NEXT STEPS
The ARTforMS innovation will continue to be used to train providers in rural MaineHealth locations and has even been demonstrated on a recent MMC service trip to Kenya. As CWRU’s augmented reality software is further refined, Michael and Mary hope ArtforMS can be expanded to accommodate larger pediatric simulation manikins and more distress scenarios.
IN THE NEWS
Portland Press Herald: New division of MaineHealth helps turn medical ideas into reality
TEAM
Michael Ferguson, MD, MTeach
Pediatric Intensivist
The Barbara Bush Children’s Hospital at Maine Medical Center
Mary Ottolini, MD, MPH, MEd
George W. Hallett, MD Chair of Pediatrics
The Barbara Bush Children’s Hospital at Maine Medical Center
Case Western Reserve University
Our Purpose
MaineHealth Innovation builds connections to drive diversity of thought, educates to produce creative problem-solvers and funds to accelerate ideas. By leveraging the ideas, insights and expertise of all care team members to develop novel solutions to our unmet care needs, we are working together so our communities are the healthiest in America.
